The Neuroscience Behind Post-Traumatic Growth from Survival to Thriving
By Dr. Kate Truitt
A client walks into your office, their shoulders tight, their breath shallow, eyes darting with every subtle noise. They share how even the most common life experiences—a ringing phone, a sudden laugh—send their nervous system into high alert. “I don’t get it,” they say. “I know I’m safe, but my body doesn’t listen.”
As mental health professionals, we recognize this experience as the survival brain working overtime. Trauma leaves an imprint on the brain, priming it to react to potential threats long after the danger has passed. But here’s the hopeful part: The brain can change. Through neuroplasticity, the brain’s natural capacity to rewire itself, we can help clients shift from survival-driven reactivity to a growth-oriented mindset.
Neuroscience is showing us that healing isn’t just possible. It’s accessible. By guiding clients to engage with practices that support neural rewiring, we empower them to move from a state of survival to one of resilience, strength, and even post-traumatic growth.
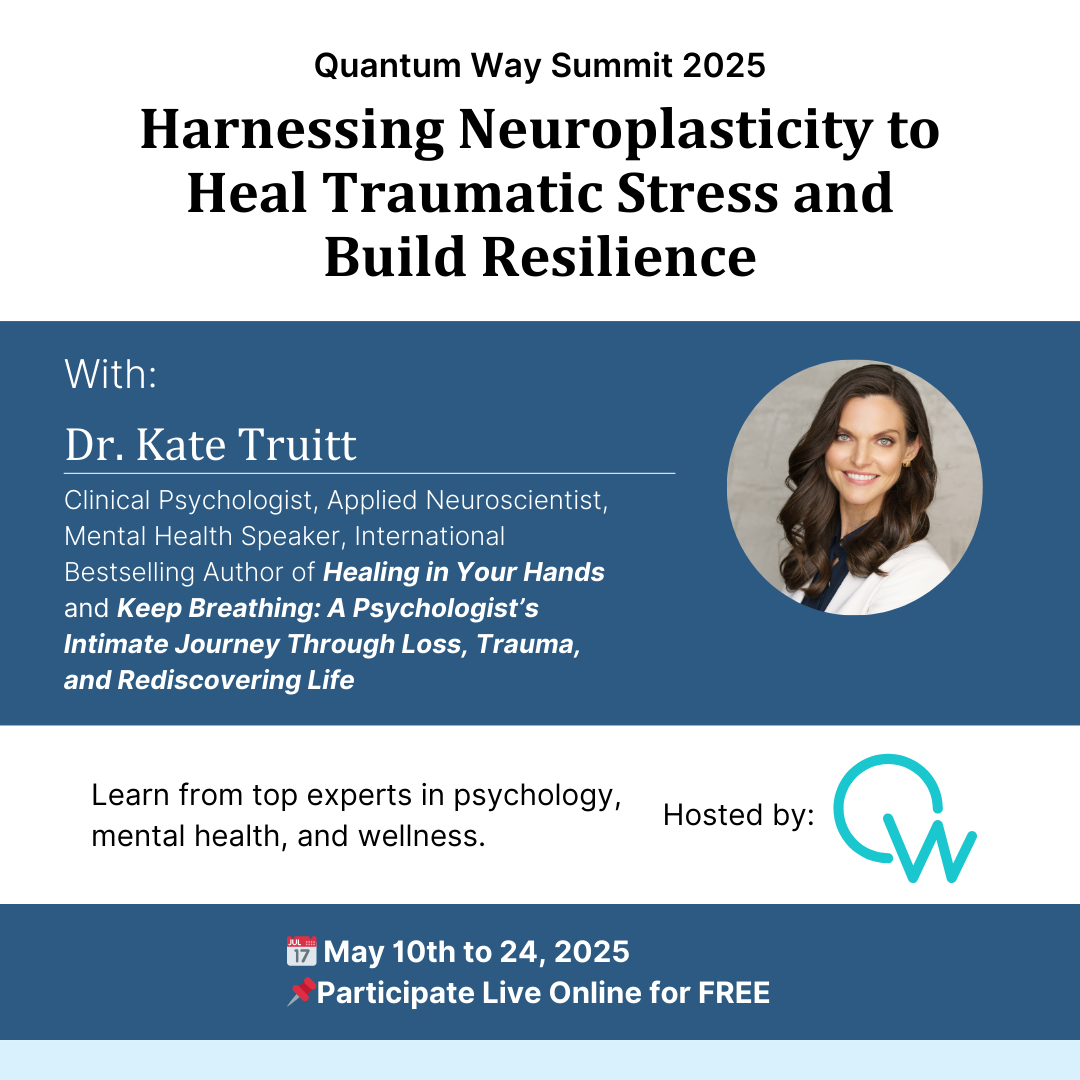
This is one of the key topics I’ll be exploring at the Upcoming Quantum Way Summit 2025, where I’ll be presenting Harnessing Neuroplasticity to Heal Traumatic Stress and Build Resilience. We’ll explore how neuroplasticity offers new hope for trauma recovery and discuss practical strategies you can implement in your practice. Registration is FREE so don’t miss it!
Trauma and Survival Mode: The Brain’s Protective Mechanisms
When clients experience trauma, their brains shift into survival mode to protect them from future harm. When Amy, the amygdala detects a potential threat, she activates the sympathetic nervous system, activating one of the 4 F’s: fight, flight, freeze, or fawn. This response happens in just 75 milliseconds which is faster than conscious thought or a blink of an eye. It’s an elegant system designed to protect us from real danger. But trauma can cause Amy to get stuck in high alert, perceiving everyday experiences as potential threats.
For example, a client who was in a car accident may feel their heart race at the sound of screeching tires even when they’re safe at home. Their amygdala has paired the sound of screeching tires with life-threatening danger, turning that sensory input into a survival trigger.
By helping clients understand the brain’s survival mechanisms, we normalize their experiences and reduce the shame often associated with trauma symptoms. When clients realize their reactions are rooted in biology, not personal failure, they can move from self-blame to self-compassion. And that self-compassion creates fertile ground for the work of rewiring the brain and cultivating post-traumatic resilience.
What is Neuroplasticity
The human brain is not a static organ. It is constantly learning, adapting, and changing in response to life experiences. This remarkable ability is known as neuroplasticity. Neuroplasticity allows the brain to reorganize itself by forming new neural connections—an innate mechanism that not only supports learning but also enables healing from trauma.
When an individual experiences trauma, the brain’s survival pathways become well-worn neural highways. These pathways are strengthened each time the brain detects a potential threat, even when that threat is no longer relevant to the present moment. For example, a person who endured childhood emotional neglect might develop a hypervigilant response to perceived disconnection in adult relationships.
However, just as the brain can learn to associate seemingly neutral experiences with danger, it can also unlearn those associations. Through intentional, repetitive practices, clients can create new, healthier pathways that prioritize safety, connection, and well-being.
From Survival to Growth: Guiding Clients Toward Post-Traumatic Growth
If there’s post-traumatic stress, there’s also post-traumatic resilience. It involves becoming stronger and wiser after trauma. Just like the phoenix, where one may burn up in the flames and rise again, individuals have the ability to create a space where they learn and grow from what has occurred. In this psychoeducational video, I discuss how neuroplasticity allows for the creation of post-traumatic resilience at a neurobiological level.
Post-traumatic growth (PTG) represents a transformative process in which individuals not only recover from trauma but also develop new perspectives, strengths, and possibilities for their lives. As clinicians, we can support clients on this journey by guiding them through the five stages of PTG:
- Initial Shock & Survival: Clients often experience fear, confusion, and disorientation immediately following trauma.
- Emotional Processing: The brain begins to make sense of what happened, often accompanied by strong emotional responses.
- Cognitive Reappraisal: Clients start to reframe the experience, exploring its meaning and potential lessons.
- Integration & New Narratives: Trauma becomes part of the client’s story without defining their identity.
- Resilience & Growth: Clients discover strengths, priorities, and possibilities they hadn’t recognized before.
Practical Strategies for Clinicians
- Psychoeducation
Trauma can feel like an invisible adversary, leaving clients confused and often ashamed of their own reactions. Psychoeducation helps demystify these responses by providing a neuroscience-based understanding of what’s happening in the brain.
When we teach clients about the amygdala’s role as the brain’s protector, they begin to see their hypervigilance, emotional reactivity, or dissociation as survival mechanisms not personal flaws. Concepts like the 4 F’s of trauma—fight, flight, freeze, and fawn—can help clients recognize how their brains adapted to past dangers and, more importantly, how these patterns can be gently rewired through neuroplasticity.
- Self-Compassion and Reframing
Shame is a common companion for trauma survivors. It can whisper insidious messages like “I’m broken” or “It’s my fault this happened.” Self-compassion and cognitive reframing provide clients with powerful tools to challenge these narratives and create new, empowering beliefs. This psychoeducational video can help connect inward and get curious about what our mind and body need to honor.
Neurobiologically, self-compassion practices activate the brain’s caregiving systems, increasing oxytocin and reducing cortisol. As clients learn to speak to themselves with the same kindness they might offer a friend, their brains begin to associate distress with comfort rather than fear.
- Guided Meditations
Trauma often disconnects clients from their bodies, leaving them feeling numb, disoriented, or perpetually on edge. Guided meditation, combined with self-havening touch, can help clients re-establish a safe, grounded relationship with their physical selves.
When clients practice guided meditation, they activate the brain’s parasympathetic nervous system, shifting from survival mode into a state of calm and safety. The intentional focus on breath, paired with gentle touch, helps reduce amygdala activation and fosters new neural connections centered on peace and presence.
The Future of Trauma Care
The field of trauma treatment is evolving rapidly, with neuroscience playing an increasingly central role in shaping clinical practices. In the past, trauma recovery often relied heavily on talk therapy alone. While narrative work remains essential, we now know that trauma lives not only in the mind but also in the body.
The integration of brain-based therapies, such as EMDR, the NeuroTriad Model, Deep Brain Re-Orienting, and neurofeedback, allows clinicians to work directly with the nervous system. These approaches help recalibrate the brain’s threat-detection systems and restore a sense of safety. As research continues to uncover the intricate relationships between trauma, neurobiology, and resilience, the future of trauma care is becoming increasingly personalized and holistic.
Some emerging trends include:
- Greater use of psychosensory interventions, such as mindful touch, to support self-regulation.
- Growing emphasis on early intervention to prevent chronic trauma symptoms.
- Expanded research on the intersection of neuroplasticity and post-traumatic growth.
For mental health professionals, staying informed about these advancements is crucial. By integrating neuroscience-informed techniques into your practice, you empower clients to move beyond survival and step into a life of resilience and growth.
I encourage you to join me at the coming Quantum Way Summit 2025 which is focused on highlighting key topics around Trauma, Attachment, and Resilience. My session, “Harnessing Neuroplasticity to Heal Traumatic Stress and Build Resilience,” will give you insights and tools you can use immediately to support clients on their journey from survival to growth. Click here to register for free.
Reference
- American Psychological Association. (2016, November). Growth after trauma: Why are some people more resilient than others—and can it be taught? Monitor on Psychology. https://www.apa.org/monitor/2016/11/growth-trauma
- Elsevier. (n.d.). Posttraumatic growth. ScienceDirect. https://www.sciencedirect.com/topics/psychology/posttraumatic-growth
- Center for Mental Health. (n.d.). Post-traumatic growth. https://www.centerformentalhealth.in/post-traumatic-growth/




















